Tuberculosis (TB)
- 2022-03-23
Tuberculosis (TB)
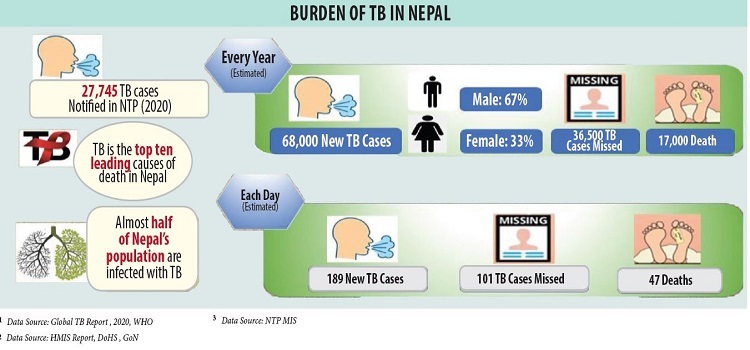
is one of the top 10 causes of death in Nepal. It is estimated that about
17,000 people die due to TB every year in Nepal. Tuberculosis is caused by a
bacterium called Mycobacterium Tuberculosis. Tuberculosis is an infectious
disease that primarily affects the respiratory system, but it can also affect
other systems, such as the gastrointestinal system, musculoskeletal system,
nervous system, etc. It may be present as a latent or an active infection.
Active cases can be presented with symptoms like cough, hemoptysis (blood in
the sputum), fever, weight loss, etc.
Usually seen in:
All age groups
Gender affected:
Both men and women but more common in men
Body part(s)
involved: Lungs, Intestine, Bones, Brain, Blood
Prevalence
Rate: Worldwide: 10 million (2019). In Nepal: According to National
Tuberculosis Prevalence Survey (2018-19), estimates 69,000 new TB cases
annually. Previously, it was estimated to be 44,000 per year. However, around
27,000 people affected with TB are diagnosed and enrolled in the treatment
every year.
Mimicking
Conditions: Pneumonia, Lung cancer, Fungal infection of the lung, Sarcoidosis
SYMPTOMS OF TUBERCULOSIS
Pulmonary tuberculosis or TB of
the lungs is the most common type of TB. Other types such as the TB of the
bones, lymph nodes, brain, kidneys, intestine, and genitals are also seen.
Symptoms of Pulmonary TB
Tuberculosis most commonly affects
the lungs and can cause the following symptoms:
Coughing that lasts for more than 2 weeks with
or without fever
Fever, especially an evening rise in body
temperature
Presence of blood in the sputum
Chest pain
Loss of appetite
Loss of weight
Chronic fatigue
Night sweats and chills
Symptoms of Systemic TB (other than pulmonary TB)
Occasionally, tuberculosis may
also affect other organs, such as bones, stomach, etc., and presents with
common symptoms like fever, weight and appetite loss and some specific symptoms
related to organ system involved like
Bone TB involving the spine can cause back pain
and neurological complications like paraplegia where the lower limbs become
paralyzed.
Gastrointestinal system disease can cause
nausea, vomiting, diarrhea, malabsorption etc.
Tuberculosis of the kidneys can cause blood in
the urine.
Infection involving the brain and its covering
membrane can cause seizures, headaches, neurological abnormalities, etc.
CAUSES OF TUBERCULOSIS
Tuberculosis is caused by a
bacterium called Mycobacterium tuberculosis. TB usually spreads from one person
to the other through the air. When a person suffering from TB sneezes, coughs
or spits, the bacteria get into the air. Hence, when a person inhales even a
few of these bacteria from the air, he/she becomes infected. Although it is
contagious, the bacteria grow at a slow rate and requires you to spend
considerable time around the person who is sick. This means, it requires close
and prolonged contact with a person who has active tuberculosis.
Note: Remember!
Tuberculosis cannot spread through a simple handshake or sharing utensils as
the bacteria cannot survive for long outside of the human body.
TYPES OF TUBERCULOSIS
There are 5 different types of
tuberculosis based on the type of infection. These include:
Latent tuberculosis
Latent tuberculosis does not cause
any symptoms as the body’s immune system keeps the infection at bay. In latent
tuberculosis, the person carries the bacteria but does not develop any symptom
However, there is a possibility that the latent infection may reactivate at a
later stage in life when the body’s immune defenses go down and may lead to
active disease.
Active tuberculosis
Active tuberculosis refers to a
condition where the bacteria are in an active stage and cause symptoms, further
classified into pulmonary and systemic tuberculosis.
Pulmonary tuberculosis is
primarily a disease of the lungs (pulmonary TB).
Systemic tuberculosis, active
tuberculosis is present in other parts of the body, such as bones, lymph nodes,
brain, kidneys, intestine, and reproductive system.
Disseminated tuberculosis
Miliary tuberculosis, this is a
severe type of infection where the tuberculosis bacteria spread to the entire
body through the bloodstream.
Multidrug resistant
tuberculosis (MDR TB)
MDR TB is caused by a bacterium
which is resistant to at least two most common and potent drugs used to treat
TB namely isoniazid and rifampin.
Extensively drug resistant
tuberculosis (XDR TB)
This is a rare type of
tuberculosis in which the bacteria are resistant to more than two drugs used to
treat TB. In addition to isoniazid and rifampin, people suffering from XDR TB
are resistant to fluoroquinolones (an antibacterial medicine) and at least one
of three injectable second-line drugs used to treat bacteria.
RISK FACTORS OF TUBERCULOSIS
Although all age groups are at
risk of TB, the risk is higher in people who:
- Live in or travel to a country with a higher
prevalence of tuberculosis such as tropical and developing countries.
- Work in places constantly exposed to crowds,
such as hospitals, community centers, prisons, etc.
- Suffer from malnourishment. It is seen that
undernourished people are 3 times more at risk of TB as compared to healthy
people.
- Suffer from diabetes or are on medicines such as
steroids or anti-cancer drug therapy.
- Suffer from weakened immunity or are recovering
from an illness.
- Are infected with HIV/AIDS as the risk of
getting tuberculosis is 18 times higher for patients with HIV.
- Consume excess alcohol and smoke tobacco
products.
DIAGNOSIS OF TUBERCULOSIS
Along with a detailed history and
physical examination, the doctor also orders laboratory tests and imaging
studies to confirm a suspected case of tuberculosis.
Following tests are used to
confirm a diagnosis:
Blood Tests
- Cartridge based nucleic acid amplification
test (CB-NAAT)
- TB Platinum Interferon Gamma
Release Assay
- Complete Blood Count, Erythrocyte
Sedimentation Rate
- Sputum AFB (ZN Stain)
- Mycobacterium tuberculosis DNA PCR
- Qualitative
- Skin prick test (Mantoux test)
Imaging studies
- In pulmonary tuberculosis cases,
imaging studies like X-Ray chest PA View, HRCT chest - plain are
required to evaluate the extent of the disease in the lungs.
- In extrapulmonary tuberculosis
cases, other imaging studies, such as X-Ray dorsal spine AP & lateral
view, MRI brain, etc., may be done as appropriate.
TREATMENT OF TUBERCULOSIS
The treatment for tuberculosis
depends on the type of infection.
Latent tuberculosis
if you have tested positive for
tuberculosis in a screening test and high-risk category, treatment may be
recommended in Nepal. The medicines for latent tuberculosis must be taken for a
duration of 6 to 9 months as prescribed by a doctor.
Active tuberculosis
Antibiotics are the main treatment
options for people suffering from TB. The treatment approach usually involves
taking these drugs for a span of several months. These medicines are usually
given in combination as part of a regimen to effectively treat tuberculosis.
These medicines kill the bacteria causing tuberculosis or prevent its growth.
The first line of treatment for
active tuberculosis consists of combination therapy with five antitubercular
drugs. Of these, streptomycin is given in the form of an injection, whereas a
single tablet consisting of all the four medicines (isoniazid, rifampicin,
pyrazinamide and ethambutol) is available. The dose of this combination
medicine is based on the weight of the patient.
Easy-to-use combination kits,
containing a combination of the first-line antitubercular drugs are also
readily available. The treatment continues for 6-8 months even if the symptoms
get better, as it ensures complete recovery and prevents the development of
drug resistance.
The DOTS (Directly
Observed Therapy - Short Term), where the patient has to take the medicine in
front of a DOTS agent. This is to ensure adherence to the treatment.
MDR TB and XDR TB
The tuberculosis bacteria are
prone to develop drug resistance. Some patients do not respond to the first
line of treatment and develop multi-drug resistant tuberculosis or MDR-TB.
There are strains of bacteria resistant to most forms of available drugs and
cause a severe form of the disease known as extensively drug-resistant
tuberculosis or XDR-TB.
Treatment options for MDR and XDR
tuberculosis consist of higher dosing of the first line of drugs and a
combination of other oral medicines and injections. The course of the treatment
is usually 18 months for MDR-TB and 224 months for XDR-TB.
Some of the common examples
include:
Amikacin injections
Streptomycin injections
Levofloxacin preparations
Moxifloxacin preparations
Para-amino salicylic acid
Clofazimine preparations
Imipenem injections
Clarithromycin preparations
Bedaquiline
SUPPORTIVE CARE
This involves use of medications
aimed to improve the symptoms such as fever, cough, and pain. Some of the
common class of drugs used for supportive care of TB are:
- Anti-fever and analgesic medicines to provide
relief from fever and pain.
- Antitussive medications to help reduce cough.
- Vitamin B supplements given along with antitubercular medicines to help combat neurological side effects like nerve pain and neuropathies caused by antitubercular medicines.
- Antacids to prevent gastro-intestinal symptoms
- Medicines to reduce uric acid level
(hyperuricemia is known to be a side-effect of TB medicines) such as
allopurinol and febuxostat are recommended.
- In some cases, an herbal medicine/tonic for the
liver is recommended as antitubercular medicines can impact the liver.
CARE FOR TUBERCULOSIS
With active tuberculosis, you can
do the following things to care for yourself at home:
- Always use a handkerchief to cover your mouth
and nose while sneezing or coughing.
- Wash your hands frequently with soap and water
or use hand sanitizers.
- Take a balanced diet rich in vitamins and
minerals.
- Drink plenty of fluids throughout the day.
- Take plenty of rest. Do not engage in any
strenuous activities.
- Take the entire course of medicines prescribed
by the doctor, even if your symptoms reduce or you start feeling better.
LIVING WITH TUBERCULOSIS
Tuberculosis is a disease that is often associated with a stigma as there are many misconceptions surrounding it. However, with recent improvements in available treatments and public awareness campaigns, the stigma of the disease is declining, and more and more people are recovering completely from the disease. In the active phase of the disease, it is advisable to refrain from interacting with many people and avoid crowded places to prevent transmission. Here are a few tips you need to keep in mind if you are on medications for tuberculosis:
- Maintain a routine if you are taking medications by yourself like taking medicines at the same time every day, marking off the date on a calendar or using a weekly pill dispenser.
- Inform your doctor if you experience any unusual
symptoms or side effects of the medications. Your doctor might consider
changing the drugs.
- Make sure you complete your course of
medications. Not finishing the course or stopping the medications mid-way can
not only increase the risk of getting sick and spreading the infection again
but can also make the bacteria resistant to the drugs.
- Do not forget to follow cough etiquettes like
covering your mouth when sneezing or coughing and throwing a used tissue in the
trash can.
- Ask your doctor about the improvement in your
condition, the change in medications, lab tests to be taken, and any questions
you have related to the condition. This will help you understand the condition
& take care of your health
- Caregivers should ensure to avoid close contact
with the patient, If possible, let the patient share a single room with proper
ventilation.
- Eat a diet rich in nutrients like vitamins, minerals, and antioxidants. Avoid eating oily, salty and spicy food. home cooked foods to boost your immunity and stay healthy.
PREVENT THE SPREAD OF TUBERCULOSIS
As tuberculosis spreads through
infected droplets, it is important for a patient with active tuberculosis to
follow certain hygiene measures to prevent the transmission of the infection.
Always cover your mouth with a
handkerchief when coughing or sneezing to prevent the spread of droplets.
Patients with active tuberculosis
must wear a surgical mask in the presence of others to prevent the transmission
of droplets.
Wash your hands with soap and
water or use hand sanitizers frequently to keep your hands clean.
The room where a patient with
active tuberculosis lives must be well ventilated and should be cleaned with a
disinfectant every day.
The pasteurization of milk also
helps to prevent humans from getting bovine TB.
The last but the most important
point is to complete your course of TB treatment because by doing so you not
only lower your risk of recurrence/remission but also prevent community
transmission of the disease.
The specialist doctors who
diagnose and treat tuberculosis are:
General physician
Chest physician
Infectious disease specialist
Respiratory specialist or pulmonologist
Related Government Center &
NGOs
National Tuberculosis Control Centre (NTCC)
SAARC Tuberculosis Centre (STC)
DOTS Centers
Nepal Anti-Tuberculosis
Association (NATA) - Stop TB
TB Nepal, NAPID Nepal, HERD and BNMT
By
Ramendra Kumar Raman, PhD, Clinical Research
References
- Barberis I, Bragazzi NL,
Galluzzo L, Martini M. The history of tuberculosis: from the first historical
records to the isolation of Koch's bacillus. J Prev Med Hyg. 2017;58(1):E9-E12.
- Tuberculosis Free Nepal
Declaration Initiative Implementation Guideline 2021/22.
- Tuberculosis. World Health
Organisation.
- Tuberculosis. Centres for
Disease Control.
- Tuberculosis. Harvard Health
Publishing.
- Diagnostic Standards and
Classification of Tuberculosis in Adults and Children. This official statement
of the American Thoracic Society and the Centers for Disease Control and
Prevention was adopted by the ATS Board of Directors, July 1999. This statement
was endorsed by the Council of the Infectious Disease Society of America,
September 1999. Am J Respir Crit Care Med. 2000 Apr;161(4 Pt 1):1376-95.
- Adigun R, Singh R. Tuberculosis. [Updated 2020 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Zaman K. Tuberculosis: a global health problem. J Health Popul Nutr. 2010 Apr;28(2):111-3.
























Leave Comment